Ulcerative colitis is an intestinal inflammatory disease that starts in the rectum and spreads out to all the sections of the colon (ascending, transverse and descending). It is a chronic disease that results in inflammation in the wall of the large intestine, known as mucosa, which works as a barrier against harmful substances and helps with secreting and carrying nutrients, water and minerals. At times, the inflammation of the mucosa extends to another layer of the colon which causes the wall to get thinner. That contributes to the likelihood of its perforation. Just like in Chron’s disease, ulcerative colitis (UC) presents periods of activity and others of remission.
Author: Adacyte
News
What is ulcerative colitis?
November 17, 2020
Patologies

UC causes the excessive apparition of ulcers, mucus and blood on the inside surface of the intestine. Those ulcers usually happen to be little and superficial. However, if they spread, they generate an accumulation of inflammatory cells. When those wounds heal, they may cause the apparition of little masses of tissue.
Besides, UC may affect other parts of the body like eyes, skin, joints… what is known as extraintestinal manifestations. That makes the patient suffer from joint pain, skin spots, stones in the gallbladder, or eye inflammation.
Just as the cause of the disease is unknown, there is no cure for it either. Nevertheless, if the symptoms are too injurious and the treatments do not work effectively on the patient, surgery may be done. It consists of reconstructing the intestinal transit with a reservoir. Another option is to remove the colon. That is considered to be the cure for the UC. Notwithstanding, it only happens after the failure of every other treatment. It is individually studied in every patient, in cases of extreme necessity.
What is the cause of ulcerative colitis?
UC arises as a consequence of a poor immune response to the organism itself. The origin of this inappropriate response is still unknown, but the stronger theories point at the genetic predisposition, the bacterial flora and the environmental influences as the possible causes of the disease.
There exist multiple harmful substances to our intestine, to which the immune system (under normal circumstances) responds properly protecting the organism from any damage that may affect it. Sometimes those intestinal immunologic responses fail and that is when the UC appears. This situation is usually prolonged and maintained in the long term, making the ulcerative colitis a chronic disease.
The reasons why those immune responses fail are still unknown, but the most powerful theories state that it could be due to genetic alterations of the intestinal immune system. Its cells have the ability to notice the presence of different pathogenic agents and they are able to stop them. Some people present genetic alterations in those agents’ receptors, which lead to wrong identifications and, consequently, to wrong inflammatory responses.
Is the ulcerative colitis hereditary?
Despite the implication of genetic factors in the apparition of the disease, it is not considered to be hereditary. That is because the external factors like tobacco, the previous gastrointestinal infections, some drugs, or even the stress have influence on it too. It does exist the hereditary influence in suffering from UC. However, it is not more than 15% of the risks for first-degree relatives.
How is ulcerative colitis diagnosed?
Diagnosing the disease is sometimes difficult, because the symptoms may be diverse and, in some occasions, they are attributed to other conditions. The blood and stool tests are the most reliable ones, they can help identify if there is inflammation or infection; the so-called image tests, where the inflamed zones may be seen, besides the extension and the seriousness of the disease. And lastly, the endoscopic tests with biopsies confirm the diagnosis of the UC. Those provide any type of necessary information in order to know if there exist ulcers, inflammation, bleeding or stenosis.
Ulcerative colitis1 is an intestinal inflammatory disease that affects the colonic mucosa (large intestine). This mucosa works as a barrier against harmful substances. It also helps secreting and transporting nutrients, water and minerals; and lubricating the inner part of the intestine in order to facilitate defecation. Its inflammation is produced because the immune system generates an inappropriate inflammatory response against the organism itself. The origin of this failure in the intestinal immune system’s responses is not fully known.
When the mucosa gets inflamed, little wounds (ulcers) appear in the inner lining of the colon. This chronic inflammation starts in the rectum and spreads out to other sections of the colon (ascending, transverse and descending). That means that the affectation may have a variable extension.
The most common symptoms of the ulcerative colitis are liquid defecations with mucus and/or blood, stomach ache, straining to defecate, fever, weight loss and fatigue. Besides, other organs like skin, eyes, bones, etc. may be affected. Most people suffering from ulcerative colitis experience from mild to moderate symptoms. There will be periods of activity when the symptoms occur (called flares). However, there are also periods of normality when the disease seems to disappear (called remission phases). Some people may experience long remission phases.
Risk factors As well as Crohn’s disease, UC is a modern age disorder. In fact, the frequency has increased in developed countries since the mid-twentieth century. This disease affects males and females approximately in equal proportions.
The risk factors may be:
- Age. Even though it may appear at any age, it generally occurs before the age of 30. Nevertheless, there are also cases in which the disease has been diagnosed after the age of 60.
- Race or ethnic origin. Although white people have a higher risk of experiencing the disease, any race can have it. If you have Ashkenazi Jewish ancestry, the risk is higher.
- Family history. It is frequent to find UC cases within the members of the same family. Between 8 and 14% of the patients with ulcerative colitis have a family history of inflammatory bowel disease. Therefore, the risk increases when you have a close relative (parent, sibling or son/daughter) who suffers from this disease.
The cause of the ulcerative colitis and other unknown issues for the science Even though science has made great efforts to find out the cause of ulcerative colitis, it is still unknown. Science still wonders what the specific cause of the inappropriate inflammatory response of the immune system is. According to GETECCU2, current researches state that the disease may appear as a result of a complex interaction of several factors.
One of those factors is a person’s genetic predisposition (susceptibility) to suffer from the disease. However, there are other factors that also seem to be the key in the appearance of the UC like the exposition to environmental factors, the intestinal commensal microflora and the possible involvement of infectious agents. It is believed that the genetic alterations affect the ability of the immune system to tolerate the commensal bacteria and the intensity of the inflammatory response against those bacteria.
Nonetheless, the genetic origin is not completely clear yet. In conjunction with this issue, there exist questions about the pathogenesis of ulcerative colitis that still pose a challenge to science. Why is the inflammation restricted to the mucus layer? Are the epithelial cells of the colon the specific aim of an immune response? How does the luminal microbiota affect the inflammatory response?
News
Ulcerative proctitis: What is it and how is it treated?
October 20, 2020
Patologies

Ulcerative proctitis is the inflammation of the lining in the inner wall of the rectum. Given that feces pass through the rectum to come out the organism, the evacuation act becomes painful for the patient. Besides, this kind of ulcerative colitis causes diarrhea, bleeding, secretion and the feeling of having the urgent need to go to the bathroom. All these symptoms can last a short time or, conversely, become chronic.
There exist numerous causes1 for a person to suffer from ulcerative proctitis. The most frequent is to suffer an inflammatory bowel disease (IBD). But there are also other factors that may cause this condition. Some motives for suffering proctitis are sexually transmitted diseases, organism immunodeficiency, bacteria like Salmonella or antibiotics that destroy the gut flora. It may also be a side effect of radiotherapy used to treat prostate and rectal cancer.
What are the symptoms of the ulcerative proctitis?
The most frequent signs of ulcerative proctitis2 are constant urge to defecate, rectal bleeding or painful depositions. The mucus discharge of the rectum, the rectal or abdominal pain and diarrhea are also typical symptoms. If you experience any one of them, it is convenient for you to visit your physician.
In order to diagnose the disease, there are three ways to proceed. The first one is to run a proctoscopy (to examine the rectum cavity using a specific tube). It is possible to examine tissue samples with it in order to identify which bacteria, fungus or viruses are causing the proctitis. Another way of knowing if a patient is suffering from this condition is to make stool and blood tests. Lastly, it is also possible to look at some sections of the intestine using a colonoscopy. That helps detect Crohn’s disease as well as ulcerative colitis and, therefore, if that kind of colitis is a proctitis.
What is the appropriate treatment for the ulcerative proctitis?
The treatment3 for this disease depends on the cause of the inflammation. If the proctitis is caused by an infection, we will need drugs to cure it. They may be antibiotics, if it is a bacterial infection; or antivirals, if it has a viral origin.
Another possibility is for the condition to be caused by radiotherapy. If the proctitis is mild, it is unnecessary to start a treatment. If the pain is acute and the bleeding is severe, it is necessary to start a treatment, either take pills, suppositories or enemas. That serves to control the inflammation and reduce bleeding. Stool softeners and dilatation can also be used, both options help release fecal loading in the intestine. Finally, using a treatment to destroy the damaged tissue is another solution. Ending with the bleeding tissue will improve the symptoms of the proctitis.
If ulcerative proctitis is caused by an inflammatory bowel disease (IBD), the aim is to reduce the inflammation of the rectum. The treatments for that are anti-inflammatory or immunosuppressive drugs. If that does not work, the last option is to surgically remove the damaged section of the digestive system.
If this disease is not correctly treated, it is possible to develop a series of complications. The patient may suffer from anemia due to the chronic rectal bleeding. This results in dizziness, fatigue, shortness of breath, head ache or pale skin. Another consequence of not treating the proctitis successfully is the apparition of ulcers in the inner rectal lining. If those spread out to the whole bowel wall, it may generate fistulas.
The ulcerative proctitis is a type of ulcerative colitis. In particular, it is a chronic inflammatory disease that consists of the inflammation of the mucosa in a certain sections of the large intestine: the rectum. It is a portion of the digestive tube situated before the anus where the feces are contained prior to leaving the organism. For it to be considered ulcerative proctitis, the inflammation should not exceed 15 centimeters of the intestinal tube from the anal sphincter. Approximately, between 30 and 40% of patients with ulcerative colitis present this location. It is also fair to say that this form of ulcerative colitis is usually the mildest.
This inflammation makes it difficult for the stool to pass, therefore, the patient will, frequently, feel pain while defecating. This pain (rectal tenesmus: pain along with a feeling of not having adequately emptied the bowels, despite the repeated practice of evacuation) may be associated or not to the mucopurulent or even hemorrhagic (hematochezia) stool discharges. However, proctitis may also cause non-painful hemorrhages or the passage of mucus through the rectum.
A very common symptom of ulcerative proctitis is the continual urge to defecate (bowel-rectum movement). Another is tenderness and mild irritation in the rectum and anal region. Serious symptoms are pus and blood in the defecation, or cramps and pain during the bowel movement. All these symptoms can last a short time or, conversely, become chronic.
How is ulcerative proctitis diagnosed?
In order to diagnose the disease, there are three ways to proceed. The first one is to run a proctoscopy (to examine the rectum cavity using a specific tube). It is possible to examine tissue samples with it in order to identify which bacteria, fungus or viruses are causing the proctitis. Another way of knowing if a patient is suffering from this condition is to make stool and blood tests. Lastly, it is also possible to look at some sections of the intestine using a colonoscopy. That helps detect Crohn’s disease as well as ulcerative colitis and, therefore, if that kind of colitis is a proctitis.
A precise diagnose of this complication implies defining the severity of the inflammation. This information provides the basis for the selection of the most appropriate treatment and the prognosis of the patient. If this disease is not correctly treated, it is possible to develop a series of complications. The patient may suffer from anemia due to the chronic rectal bleeding. This results in dizziness, fatigue, shortness of breath, head ache or pale skin. Another consequence of not treating the proctitis successfully is the apparition of ulcers in the inner rectal lining. If those spread out to the whole bowel wall, it may generate fistulas.
What is the appropriate treatment for the ulcerative proctitis?
The ulcerative colitis is the most frequent cause of the ulcerative proctitis, but it is not the only one. There are other factors that may cause this condition. Some motives for suffering it are sexually transmitted diseases, organism immunodeficiency, bacteria like Salmonella or antibiotics that destroy the gut flora. It may also be a side effect of radiotherapy used to treat prostate and rectal cancer. The treatment for this disease depends on the cause of the inflammation.
If ulcerative proctitis is caused by an inflammatory bowel disease (IBD), the aim is to reduce the inflammation of the rectum. The treatments1 for that are anti-inflammatory or immunosuppressive drugs. If that does not work, the last option is to surgically remove the damaged section of the digestive system.
If the proctitis is caused by an infection, we will need drugs to cure it. They may be antibiotics, if it is a bacterial infection; or antivirals, if it has a viral origin. Another possibility is for the condition to be caused by radiotherapy. If the proctitis is mild, it is unnecessary to start a treatment. If the pain is acute and the bleeding is severe, it is necessary to start a treatment, either to take pills, suppositories or enemas. That serves to control the inflammation and reduce bleeding. Stool softeners and dilatation can also be used, both options help release fecal loading in the intestine. Finally, using a treatment to destroy the damaged tissue is another solution. Ending with the bleeding tissue will improve the symptoms of the proctitis.
News
What does having positive calprotectin mean?
September 22, 2020
Patient

Fecal calprotectin 1 (FC) is a protein found in leucocytes, and it appears in the intestinal mucosa when there is inflammation. It can be detected in the stool. If a patient’s test results show positive calprotectin, it means that there is intestinal inflammatory activity. This biomarker allows assessing that activity in an easy, fast and non-invasive way.
The FC varies its presence levels in the organism depending on the age. Newborns have elevated levels, but it decreases from the first week of life to the age of 5, when they are equal to those of an adult.
It is very useful to diagnose the inflammatory bowel disease (IBD), as well as to evaluate the response to the treatment and to see what course ulcerative colitis or Crohn’s disease take. As the positive calprotectin means that there is activity, the subsequent fall of it means the treatment is working well.
In order to detect fecal calprotectin, just take a stool sample and put it in a container. It is a normal collection that does not require any particular care. It is the same process as for a routine urine test; it is advisable to take the sample with the first deposition of the day. It can be stored for three days maximum before taking it to the corresponding specialist for it to be analyzed.
It is not recommended to administer treatments such as suppositories or enemas within 24 hours prior to the collection of the sample. Neither is to take anti-inflammatory drugs within the previous days. And lastly: if there is a scheduled colonoscopy, the collection cannot be done until three days after the test.
The increase 2 in calprotectin occurs three months before experiencing the disease again after an effective treatment. This can serve to foresee the risk, although, in some occasions, that increase just implies activity without symptoms.
Positive calprotectin: diagnose for an IBD
It is not completely effective to use the digestive symptoms as the only filter for the indication of a colonoscopy. Those are quite frequent and not specific whatsoever, because they are not exclusive signs of an inflammatory bowel disease.
Positive calprotectin may be a first test to identify an organic bowel disease before conducting a colonoscopy or a radiological study. This is very important in children, because avoiding a test like colonoscopy is best for them. In the case of short age patients experiencing persistent abdominal pain and sudden changes in their usual way of evacuating, it is almost certain that the positive calprotectin implies the presence of IBD. The use of this biomarker in the initial diagnosis of children could lead to an improvement in the referral to the endoscopic units.
It is common for doctors to find it difficult to differentiate between an irritable bowel syndrome (IBS) and an inflammatory bowel disease (IBD). That happens because sometimes symptoms are practically the same (diarrhea and abdominal pain) for IBS and IBD. Fecal calprotectin comes into play here, since its level is higher in IBD patients than in those suffering from IBS.
Positive calprotectin, valid to predict relapse
Fecal calprotectin (FC) is a protein found in leucocytes, and it appears in the intestinal mucosa when there is inflammation. It can be detected in the stool. If a patient’s test results show positive calprotectin, it means that there is intestinal inflammatory activity. This biomarker allows assessing that activity in an easy, fast and non-invasive way.
The FC varies its presence levels in the organism depending on the age. Newborns have elevated levels, but it decreases from the first week of life to the age of 5, when they are equal to those of an adult.
It is very useful to diagnose the inflammatory bowel disease (IBD), as well as to evaluate the response to the treatment and to see what course ulcerative colitis or Crohn’s disease take. As the positive calprotectin means that there is activity, the subsequent fall of it means the treatment is working well.
In order to detect fecal calprotectin, just take a stool sample and put it in a container. It is a normal collection that does not require any particular care. It is the same process as for a routine urine test; it is advisable to take the sample with the first deposition of the day. It can be stored for three days maximum before taking it to the corresponding specialist for it to be analyzed.
It is not recommended to administer treatments such as suppositories or enemas within 24 hours prior to the collection of the sample. Neither is to take anti-inflammatory drugs within the previous days. And lastly: if there is a scheduled colonoscopy, the collection cannot be done until three days after the test.
The increase in calprotectin occurs three months before experiencing the disease again after an effective treatment. This can serve to foresee the risk, although, in some occasions, that increase just implies activity without symptoms.
Positive calprotectin: diagnose for an IBD
It is not completely effective to use the digestive symptoms as the only filter for the indication of a colonoscopy. Those are quite frequent and not specific whatsoever, because they are not exclusive signs of an inflammatory bowel disease.
Positive calprotectin may be a first test to identify an organic bowel disease before conducting a colonoscopy or a radiological study. This is very important in children, because avoiding a test like colonoscopy is best for them. In the case of short age patients experiencing persistent abdominal pain and sudden changes in their usual way of evacuating, it is almost certain that the positive calprotectin implies the presence of IBD. The use of this biomarker in the initial diagnosis of children could lead to an improvement in the referral to the endoscopic units.
It is common for doctors to find it difficult to differentiate between an irritable bowel syndrome (IBS) and an inflammatory bowel disease (IBD). That happens because sometimes symptoms are practically the same (diarrhea and abdominal pain) for IBS and IBD. Fecal calprotectin comes into play here, since its level is higher in IBD patients than in those suffering from IBS.
Positive calprotectin, valid to predict relapse
Relapse means experiencing the disease again shortly after finishing the convalescence of the same disease. IBD is characterized by periods of activity remission, with corresponding relapses when the intestinal inflammation increases again. This situation is difficult to predict. It is usually done by monitoring the patient to explore symptoms, although this is not fully effective. The signs may appear after the inflammation of the mucosa; therefore, it does not serve to detect relapses. Fecal calprotectin is more sensitive to detect the risk of relapsing.
Calprotectin is an abundant protein in the organism that comes from leucocytes (white blood cells). That is, it is a substance produced in the immune system cells which helps the body fight off infections and diseases. When there is inflammation in the gastrointestinal (GI) tract, neutrophils move to the inflamed area and that is when they liberate the calprotectin. A posteriori, those proteins will be eliminated along with other residues as stool. The fecal, in the stool, concentration of calprotectin is about 6 times higher compared to the levels of it in blood.
The stool, when it is examined under the microscope in the laboratory, will show levels of positive calprotectin. As a general rule, high levels of calprotectin indicate bacterial or parasitic infections, colorectal cancer or certain diseases that cause intestinal inflammation, such as ulcerative colitis and Crohn’s disease. In those latter cases, the higher the calprotectin, the more severe the inflammation. However, fecal calprotectin does not indicate the location or the cause of the gastrointestinal inflammation. In order to determinate the cause, signs and symptoms of the inflammation a colonoscopy can be required.
Low levels of calprotectin indicate that the signs and symptoms are attributable to a different cause (non-inflammatory). That is the case for irritable bowel syndrome and viral infections. Precisely, it is common for doctors to find it difficult to differentiate between an irritable bowel syndrome (IBS) and an inflammatory bowel disease. That happens because sometimes symptoms are practically the same (diarrhea and abdominal pain) for both diseases. Fecal calprotectin comes into play here: this biomarker will show higher levels in IBD patients than in those suffering from IBS.
Positive calprotectin in the IBD monitoring
Those who join the growing tendency to base the treatment of inflammatory bowel disease on objective data, propose to identify biomarkers that allow selecting those patients who will benefit more from an endoscopic examination. The fecal calprotectin has been proposed here as a biomarker for the bowel inflammation. It allows differentiating the IBD, it has a better correlation with the degree of inflammation than clinical indices and serological markers, and could be useful for predicting mucosal healing and risk of relapse. Because, with the measurement of calprotectin in stool repeatedly, changes can be monitored at the intestinal level of a patient for a long period of time.
Relapsing means experiencing the disease again shortly after finishing the convalescence of it. IBD is characterized by periods of activity remission, with corresponding relapses when the inflammation increases again. This situation is difficult to predict. It is usually done with patient’s monitoring to explore symptoms, although this is not fully effective. The signs may appear after the inflammation of the mucosa; therefore, it does not serve to detect relapses.
The fecal calprotectin is said to be more useful to discover the risk of relapsing. Since, the increase1 in calprotectin occurs three months before experiencing the disease again after an effective treatment. This can serve to foresee the risk (although, in some occasions, this increase just implies activity without symptoms).
What is necessary for the realization of a fecal calprotectin?
In order to detect fecal calprotectin, just take a stool sample and put it in a container. The test can be reliably analyzed on a sample of less than 5 grams, although it is recommended for the collected sample to be larger. It is a normal collection that does not require any particular care. It is the same process as for a routine urine test; it is advisable to take the sample with the first deposition of the day. It can be stored for three days maximum before taking it to the corresponding specialist for it to be analyzed.
It is not recommended to administer treatments such as suppositories or enemas within 24 hours prior to the collection of the sample. Neither is to take anti-inflammatory drugs within the previous days. And lastly: if there is a scheduled colonoscopy, the collection cannot be done until three days after the test.
- https://www.educainflamatoria.com/calprotectina-fecal-colitis
- https://www.elsevier.com/es-es/connect/educacion-medica/niveles-de-calprotectina-fecal,-claves-para-el-diagnostico-y-tratamiento-de-la-eii-conclusiones-del-ii-elsevieraegtalks
- Faecal calprotectin | Testing & causes of high result (ibdrelief.com)
News
Five keys to a proper diet if you have ulcerative colitis
July 21, 2020
Patologies

Ulcerative colitis is a chronic disease that has no cure. It is essential to follow a proper diet1 in order to help improve patient’s quality of life. The damage to the intestine from inflammation and the ulcers related to the pathology can affect the levels of some minerals. This implies a much higher risk of experiencing anemia, osteoporosis, low defenses, premature aging, nervousness or fatigue. All this added to a possible lack of vitamins, makes it essential for the patient to consider what can be eaten with ulcerative colitis.
There is no evidence that feeding causes, prolongs or worsens a flare. The main objective2 of following a proper diet is to avoid patient’s malnutrition. The causes of this possible malnutrition can be very varied: a greater need of energy ought to inflammatory activity, fever or corticoids. The loss of proteins and other digestive components are also factors, which happens because of the diarrheas and the bleeding characteristic of the disease.
Ulcerative colitis (UC) patients usually lose weight, due to the decreased appetite and the tissue degeneration during flares activity. It is necessary to ensure the supply of proteins and calories to the organism. Especially, it is necessary in children and teenagers in order to avoid a delay in their development and growth. Furthermore, it is important to take some UC patients’ allergies and intolerances into account. This must be like that in order to help the flare remission and improve bowel tolerance. When the inflammatory activity manifestation ends, a temporary lactose or fat intolerance may remain in the organism.
It is important to follow an immunostimulant diet and provide the micronutrients of which the absorption has been reduced by the inflammatory bowel activity, such as zinc, selenium and vitamins A, C and E. It is also necessary to be aware of the intestinal transit to balance the episodes of diarrhea and constipation.
What can you eat with ulcerative colitis?
The most important is to keep in mind that it does not exit a standard diet that works for each and every ulcerative colitis patient. Depending on each personal situation one type of food or another is advised, but there are general recommendations.
There are two different phases of the disease. There is the flare3 phase, when the diet is different from the one suggested during the activity remission phase. In the latter case, the recommendations are the same for everybody. It is all about following a balanced diet, knowing that certain foods may make you feel sick. This depends on each patient individually, and is checked by introducing new meals to know if they are tolerable. If we introduce a substance for two or three days and it does not cause any change in our body, it means that we can incorporate it into our diet. Nonetheless, if this food causes diarrheas or abdominal pain, it will be necessary to repeat the test after two weeks. This is done to ensure that that food is the one that causes us discomfort or damage in the organism.
Those are the five keys that would help you know what to eat with ulcerative colitis during a flare of the inflammatory bowel activity:
First of all, it is very important for the patient to know what foods and drinks are harmful4 during a flare. There are some foods that increase symptoms like diarrhea, abdominal pain or constipation. Keeping a written record of which substances affect the patient, positively and negatively, may help.
The second key is to eat several times a day and to do so in a relaxed way. Always eat small amounts, chew well and breathe properly. It is fundamental not to feel stressed during the food intake and to be able to do so without haste. The ideal is to eat small amounts five or six times a day. It is also advisable to stay seated for half an hour after each main meal (especially, lunch and dinner).
The third piece of advice is to drink enough. Like food, liquids should be taken in reduced amounts. Caffeine, theine, alcohol and carbonated drinks must be avoided. Drink water or hydrating drinks purchased in a pharmacy. Finally, it is necessary to balance the amount of liquids taken to the amount lost with depositions.
Fourthly, we must try to avoid eating greasy, fried, coated or breaded foods. Pastries, nuts and stews should also be removed from the diet. It is advisable to take cereals that help easy digestion and restrict the fibers intake. You have to give the necessary proteins and calories to the organism, but without exceeding.
Eventually, meals should be steamed, boiled, grilled or cooked in their juice. This helps to better maintain nutrients and vitamins that are present in substances. Dishes should be seasoned with salt, unless the doctor says otherwise. Food should be taken lukewarm, neither very cold nor very hot. Fruits, vegetables, milk and its derivatives and legumes should be introduced gradually. If those make you feel sick, take them off your diet and try to include them again after a while.
- https://www.dietacoherente.com/consejos-alimentacion-en-la-colitis-ulcerosa/
- https://www.accuesp.com/que-dieta-seguir-con-eii
- https://www.educainflamatoria.com/si-se-esta-en-una-fase-activa-se-tiene-que-seguir-una-dieta-especial
- https://www.saludigestivo.es/enfermedades-digestivas-y-sintomas/colitis-ulcerosa/#recomendaciones-nutricionales
News
Remission of inflammatory diseases
June 17, 2020
Patologies

What does remission of inflammatory diseases mean?
Multiple sclerosis, rheumatoid arthritis or inflammatory bowel disease (IBD) are pathologies with shared characteristics. One of them is that we are talking about incurable diseases that occur with periods of outbreaks and others of remission. Meaning that one of their main characteristics is that the patient will go through periods of relapse when his disease will be active and others when the symptoms will improve or decrease significantly. Thus, the remission in inflammatory diseases, such as IBD, means that the pathology exists, but that that there are no symptoms.
Concretely, the Inflammatory Bowel Disease manifests with the appearance of intestinal symptoms like diarrhea, stool mixed with blood and abdominal pain. It can also present extra-intestinal symptoms such as fatigue, weight loss and joint pain. This picture will appear during a period of “outbreak”. This, also called “exacerbation” or “recidivism”, is defined as the combination of symptoms referred by the patient or objectified by a doctor of an inflammatory event. An outbreak must last, at least, 24 hours and occur in the absence of fiver or infection. The interval between two different outbreaks may not be less than one month. A sharp worsening of a previous deficit is also considered an outbreak.
Remission of inflammatory diseases: When there is no trace of IBD
Remission in inflammatory diseases is a state in which symptoms are under control. This allows the patient to maintain a good quality of life, as nothing will interfere negatively with his routine. In other words, problems such as having to go to the bathroom frequently disappear temporarily, an issue faced by patients with Crohn’s disease and ulcerative colitis and which limits and affects them in the development of their daily work activities, leisure, family and social relations.
Talking about remission is possible thanks to the appearance of pharmacological therapies. These medications focus on achieving and maintaining the remission of the disease. At the same time, they prevent complications and normalize patients’ quality of life. However, the latter has a great responsibility in terms of adherence. Lack of adherence to treatment has been proven to be a significant predictor of relapse. Thus, in patients with IBD in remission who do not comply with treatment, the likelihood of regression increases more than 5 times compared to those who do so.
Treatments to improve inflammatory diseases’ remission.
There are two types of treatments for IBD: the treatment to control symptoms during outbreaks and the maintenance treatment during remission to prolong the inactivity of the inflammatory disease. Taking the drugs and following the health recommendations helps to improve the symptoms to the point of almost making them disappear.
Nevertheless, it is estimated that only half of the patients are fully adherent to treatment. This, possibly, happens because the absence of symptoms makes the person in question to forget his illness and relax. In fact, one of the most common questions doctors face is whether to stop or reduce the dose once remission in IBD is achieved. This is the main factor in the occurrence of regression. Therefore, improving adherence to treatment has become a major challenge when effectively dealing with IBD.
The decision to withdraw a drug should be made individually and always by consensus between doctor and patient, based on patient preferences, disease markers and taking into account possible relapses.
News
Ulcerative colitis treatment for steroid-dependent patients with previous failure to biologics: Adacolumn®
May 19, 2020
Product

Those patients suffering from active ulcerative colitis who meet the criteria of being steroid-dependent and not responding or being intolerant to biologics have very limited treatment options. That is the reason why the apparition of safer and more effective alternative therapies to treat the ulcerative colitis is an urgent need for this collective.
Treatment for ulcerative colitis: steroids and biologic therapy
Ulcerative colitis affects between 2.5 to 3 million people in Europe and, principally, to the young population. Half of them1 need a steroid treatment to control severe or moderate outbreaks. And, up to 40%, of them relapses whilst reducing the dose or shortly after finishing the treatment. That is known as steroid- dependent patients with ulcerative colitis.
This steroid treatment is very effective to control the symptoms of an inflammatory bowel disease outbreak. It has important advantages such as, its power (more than 80% of cases respond to steroids). Besides, they are cheap, can be administered orally in most cases, and can be used as an initial treatment for IBD cases where we still need to evaluate which definitive treatment to use.
However, the steroid treatment has important disadvantages. Firstly, they are not effective as a maintenance treatment. But, apart from that, they also have quite frequent side effects (approximately 1 out of 3 patients) and, sometimes, those are severe. Moreover, in the long term, the steroids do not modify the course of the disease. Those drugs increase the risk of suffering infections too.
Those disadvantages force the professionals to look for alternative treatments for the ulcerative colitis until achieving its remission. The TNF inhibitor drugs have been a crucial step forward here. They are indicated in patients suffering from Crohn’s disease or ulcerative colitis with a moderate-severe outbreak who do not respond favorably to conventional treatments or who present intolerance and/or contraindications to steroids or immunosuppressant therapies. However they are neither risk- free. In addition, complete remission is not achieved in more than 40% of cases2.
Alternative treatments for ulcerative colitis: leukocyte apheresis
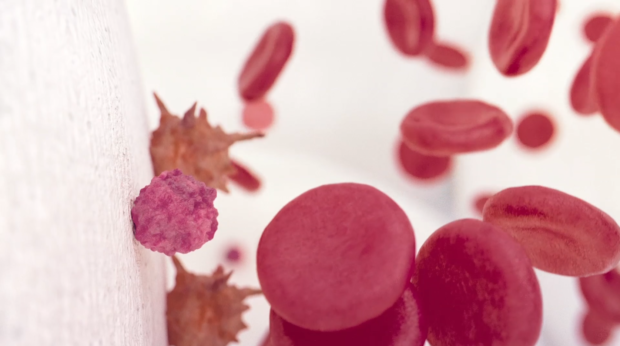
Leukocyte apheresis is a non-pharmacological treatment based on a technique that separates blood components, removing the activated leukocytes that play a role in the inflammatory process. The treatment regimen in the ulcerative colitis treatment is usually 5 to 10 weekly sessions of one hour.
Within this technique, there are two different systems:
- Centrifugation. A lymphocyte-rich fraction is removed after centrifuging a significant volume of the patient’s plasma.
- Adsorption. Blood passes through a column or filter where various leukocyte subpopulations are adsorbed. In this case, the most used device in the treatment of ulcerative colitis is the Granulocyte/Monocyte Apheresis (GMA) System with Adacolumn, whose use has been approved in the European Union since 2001.
Mode of action of Adacolumn
The medical device Adacolumn is a column formed by cellulose acetate beads bathed in saline where granulocytes (65%), monocytes (55%) and lymphocytes (2%) are selectively adsorbed. When the blood passes through it, the granulocytes, the monocytes/macrophages and the leukocytes that favor IBD adhere to the cellulose acetate spheres through the activation of the complement cascade and are removed from the bloodstream.
By reducing the amount of leukocytes in the circulatory system, non-activated young leukocytes without the ability to migrate to the inflammatory focus are mobilized from the bone marrow. In addition, an immunomodulation phenomenon occurs and, secondarily, there is also a decrease of the inflammatory infiltrate and the tissue damage3.
A Safe and effective treatment for ulcerative colitis
The treatment of ulcerative colitis in steroid-dependent patients with the GMA technique has several benefits:
- Saves steroids: the combination of steroids with apheresis favors the remission of the disease using a lower dosage and, therefore, limiting their side effects. That is the reason for it to be the best scenario to apply this technique.
- It has an excellent safety and efficacy profile.
And precisely regarding this last point, several studies have been carried out in order to verify whether those conditions are satisfied. In fact, as of 2016 there is already talk of Adacolumn proving to be an effective non-pharmacological treatment for patients with ulcerative colitis. And some studies highlight that it has proven to be extremely safe in records of clinical practice.
Studies on Adacolumn in the treatment of ulcerative colitis
Treatment with prednisone and GMA
Another research, the ATICCA1 study, aimed to evaluate the efficacy and safety of the addition of GMA to a conventional treatment for ulcerative colitis of oral prednisone in patients who meet one of the conditions we are talking about: be steroid-dependent.
Specifically, the research focused on checking the differences between a conventional oral prednisone treatment and another one in which seven GMA sessions are added, gradually reducing steroid medication over 9 weeks. The main conclusion is that the combined treatment delayed the clinical relapse and was associated with a higher rate of remission in patients who had not been treated with thiopurine.
Treatment with TNF inhibitors and GMA
Like the previous study, we found another analysis5. This time, it was developed to test the effectiveness and safety of the combination of GMA with TNF inhibitors. Likewise, the results show that it is a safe and effective treatment after the loss of response to biological agents with a significant reduction in the clinical activity of the disease and the biomarkers.
In conclusion, these data show that the quality of life of patients suffering from steroid-dependent ulcerative colitis and with previous failure to biologics improved significantly and that the intensity of most mild to moderate adverse events was reduced with Adacolumn.
BIBLIOGRAPHY
*1 Addition of Granulocyte/Monocyte Apheresis to Oral Prednisone for Steroid-dependent Ulcerative Colitis: A Randomized Multicentre Clinical Trial. February 27, 2018. Journal of Crohn’s and Colitis, 2018, 687–694. https://academic.oup.com/ecco-jcc/article/12/6/687/4911562
*2 Rutgeerts P, Sandborn W, Feagan B, Reinisch W, Olson A, Johanns J, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462-2476. https://www.gastrojournal.org/article/S0016-5085(06)02207-4/pdf
*3 José Luis Cabriada. Aféresis en enfermedad inflamatoria intestinal. ¿Una opción válida?. Gastroenterol Hepatol. 2012;35(1):22-31. https://www.elsevier.es/es-revista-gastroenterologia-hepatologia-14-articulo-aferesis-enfermedad-inflamatoria-intestinal-una-S0210570511003712
*4 Safety and Efficacy of Granulocyte/Monocyte Apheresis in Steroid-Dependent Active Ulcerative Colitis with Insufficient Response or Intolerance to Immunosuppressants and/ or Biologics [the ART Trial]: 12-week Interim Results. Journal of Crohn’s and Colitis, 2016, 1–9. https://academic.oup.com/ecco-jcc/article/10/7/812/2392090
*5 Granulocyte–monocyte apheresis: an alternative combination therapy after loss of response to anti-TNF agents in ulcerative colitis. Scandinavian Journal Of Gastroenterology. Volume 54, issue 4, april 2019. https://www.tandfonline.com/doi/abs/10.1080/00365521.2019.1600715?journalCode=igas20
News
Forum on ulcerative colitis
April 21, 2020
Patient

When we talk about the Internet, do we think of a valuable source of medical information that allows access to effective health education? Do we think of a place where professionals and researchers can promote the exchange of scientific information? Or do we consider the Internet to be a media riddled with unfounded rumors or forums with dangerously inaccurate health information? Without a doubt, on the Internet there is a lot of rigorous health information endorsed by professionals. The problem arrives when we try to separate the wheat from the chaff.
Fake news, biased information and unfounded rumors are circulating on the web at such a speed that, in a few minutes, they “have infected” millions of people. This happens, specially, in forums. We talk about open spaces to discuss specific topics created for groups with common interests to interact by exchanging ideas, theories and opinions. In them, anyone is free to give his opinion. Without filters.
In this post we will give advice to reach a forum on ulcerative colitis containing rigorous information. This is the case of EducaInflamatoria, (https://www.educainflamatoria.com/enviar-pregunta/categories/listings/colitis-ulcerosa). In this forum the health professionals who are specialists in Inflammatory Bowel Disease (IBD) themselves respond to the existing doubts.
Internet, patients and health professionals
Internet is the most important, instantaneous and economical source of information available today. The possibilities it offers its users in terms of variety of services are unlimited. The health field is no less. Internet has become an essential working tool for health professionals. It allows them to communicate with each other, to train and to update.
As for patients, Internet has allowed them to be better informed about their illness and to be able to contact people who are going through the same process as them. This, according to several studies, leads to better treatment outcomes, better use of health service resources, and a stronger doctor-patient relationship.
However, health information on the Internet can be misleading or misinterpreted. According to the II Health Unfounded Rumors Study, https://saludsinbulos.com/wp-content/uploads/2019/11/es-II-estudio-bulos-salud.pdf 63% of health professionals surveyed say that they have seen patients concerned about a health-related unfounded rumor.
6 keys to know if the forum on ulcerative colitis is reliable
When we do a search on the Internet, besides having some idea of how search engines work to find the best result and the most reliable, we must recognize when information is truthful and reliable.
Both forums and websites dealing with health issues must meet some requirements to be considered reliable. This infographic by #FFPacientes (https://ffpaciente.es/2017/03/la-salud-en-internet-cuidado/) provides some advice to help identify whether a forum on ulcerative colitis is reliable or not.
We have compiled 6 keys that shed some light on the shadows that circulate in the web:
- Anonymity: The forum must not be anonymous. In other words, the identity of the author or those responsible for the forum on ulcerative colitis must always be visible: name, medical specialty, workplace, etc.
- Professionalism of the authors: those who sign or endorse the answers to questions, comments or doubts must be medical professionals and facilitate the verification that they really are.
- Regular updating of content: In the health sector, progress is continuous. If the forum has not been updated for months the latest updates and advances in the treatment of ulcerative colitis or those related to medical protocols may not be collected.
- Promises: If the forum on ulcerative colitis proposes home remedies to cure the disease, is advertised as an alternative to medical consultation, recommends treatments without consulting a doctor or promises impossible results, it is not a place of trust.
- Image: Even if the forum is well written or has a good image or design it doesn’t mean it is a space with truthful and reliable information.
- Legal section: It is an indispensable element to know how the forum leaders will process the data and information provided by the users.
Conclusion
Remember: even if all the points mentioned above are met, the information you find in a forum on ulcerative colitis can NEVER replace the opinion of your healthcare professional. After all, he is the one who knows your personal case. That’s why he is the best person to help you and solve your doubts.
News
GEDII 2020
February 18, 2020
Events

Cascais has been for a few days the Portuguese capital of Inflammatory Bowel Disease. The city has hosted the last Annual Meeting of the Portuguese Inflammatory Bowel Disease Study Group (GEDII 2020). From 22 to 24 January, professionals from different countries who are dedicated to the study of these diseases gathered here to share experiences, exchange knowledge, and learn about new approaches to ulcerative colitis and Crohn’s disease.
As part of our commitment to help the healthcare professionals to reduce inflammation in patients with Ulcerative Colitis, Adacyte Therapeutics has not missed the appointment. During two intense days we have worked to make known the clinical benefit and the safety profile of Adacolumn. This non-pharmacological treatment has been proven to reduce the inflammation by removing leukocytes from the blood circulation. This reduces the inflammatory load without the risk of experiencing the side effects attributed to medicines. Our team has attended mainly to young and veteran doctors, gastroenterologists, pediatricians, surgeons and nurses.
GEDII 2020 Meeting Content
This interdisciplinary meeting was attended by many other profiles of professionals, both national and international. The first day of GEDII 2020, the second edition of the Educational Workshop organized by Young GEDII took place. It has also been the chosen day to celebrate the Advanced Course on perianal Crohn’s disease. On this occasion, the multidisciplinary approach required by the topic has been highlighted. As in previous editions, nursing has also been given a prominent place. The Nursing Meeting has been dedicated to the main role of the Gastroenterology Day Hospital which is so necessary in addressing IBD.
Finally, from the second day, the main meeting was held. In this meeting the specificities of pediatric pathology, the problem of comorbidities, the developments in the field of new medicines and, last but not least, the new therapeutic strategies were addressed. The microbiome, an expression of a promising future for our patients, took a place of honor.
Contact UsFor more information
Contact Us