Ulcerative colitis is a chronic disease that, well controlled, allows the patient to have a good quality of life. Therefore, having a diagnosed inflammatory bowel disease does not imply a direct recognition of disability. However, there are cases in which the patient cannot develop a normal academic, working or social life because his illness is permanently or intermittently active. This is when we talk about disability due to ulcerative colitis.
Author: Adacyte
News
Is ulcerative colitis a cause of disability?
August 24, 2022
Patologies

Disability is recognized as an objective means of quantifying the impact a disease has on everyday life. It is defined by the WHO (World Health Organization) as “any restriction or lack of capacity to perform an activity in a manner considered normal”.
Types of disability according to the severity of ulcerative colitis
Disability can be classified as transitory or temporary, or permanent and irreversible. Temporary disability refers to a transitory disability that occurs when the patient suffers an outbreak. In other words, we talk about temporary disability when a patient suffers a serious outbreak1 because his disability lasts until the symptoms subside.
On the other hand, permanent disability occurs when the negative impact on the quality of life is continued over time. Cases in which the patient does not suffer irreversible injuries also acquire this entity. This would also be the case for patients who do have post-surgery sequelae or other complications where the changes are irreversible.
How to measure the influence of disability on the patient’s quality of life?
The patient’s perception of the impact of ulcerative colitis on his quality of life is quantifiable. It is measured through Health-Related Quality of Life (HRQOL). This instrument makes available to the doctor instructions for completing the HRQOL2 questionnaire, a series of items (questions) and response options. These items are usually grouped into dimensions that measure various aspects of health, such as physical, mental and social function.
The completion of the test by the patient makes it possible to evaluate the signs and symptoms of the pathology. It also assesses the limitation or alteration of the patient’s psychological well-being, physical capacity and social activities caused by ulcerative colitis. The patient’s responses are scored to get an overview of his condition or quality of life. Thanks to them, healthcare professionals can improve the well-being of patients with ulcerative colitis3.
Is it possible to prevent disability due to ulcerative colitis?
Given the possibility of developing a disability due to ulcerative colitis, either permanent or temporary, the best prevention is a correct control and follow-up of the disease. Hence the importance of attending established medical visits, following the guidelines indicated in the consultation and maintaining the therapeutic adherence to the treatment prescribed by the doctor When the ulcerative colitis is controlled, the inflammation of the intestinal mucosa disappears; that is, the disease is in remission4. With it, in most cases, the disability also disappears. In fact, in a recent study where patients with ulcerative colitis were treated with a TNF inhibitor antibody and fully responded to the treatment were at a lower risk of developing a disability than those with no clinical response5.
The psychological aspect and the feeling of having emotional support is also essential to help the patient reduce the likelihood of suffering a disability due to ulcerative colitis. Hence, in addition to the patient’s environment, patient associations, such as those of the ACCU Confederation in Spain6, have a decisive role when the patient has to face diagnosis, treatments or, even, to maintain an adequate therapeutic adherence.
In these groups, patients share their experiences with others who are in the same situation or who have already overcome it. Information is also provided on the illness and the care services available to them and they even carry out activities with patients and their relatives.
News
Causes of ulcerative colitis: What factors trigger the disease?
August 8, 2022
Patologies

When a person is diagnosed with a chronic disease such as ulcerative colitis, they often feel vulnerable, confused, and worried. These feelings and concerns are not just about their own health or their future. It often raises serious concerns about the potential impact of this disease on their offspring. That is why, in the process of learning to live with the disease, patients often need to know the causes of the disease.
In the case of ulcerative colitis, science does not yet have a clear answer. The causes of ulcerative colitis are not known. That is, the specific cause of the inadequate inflammatory response of the immune system in the intestinal mucosa is unknown. However, the researchers are determined to provide an answer to this question. Several studies suggest that the appearance of ulcerative colitis1 may be the result of a complex interaction between various genetic and environmental factors.
Is it genetic predisposition? The causes of ulcerative colitis pointed out by science
Under normal conditions, the intestinal immune system is exposed to many potentially harmful substances and commensal bacteria that are part of our intestinal flora. The immune system is responsible for maintaining a stable balance between intestinal tolerance responses to commensal bacteria and inflammatory responses to pathogens.
However, sometimes there are failures in these responses. Inappropriate and exaggerated responses to bacteria whose presence should be tolerated are triggered. This marks the onset of the disease. Therefore, science considers that ulcerative colitis may be the result of a rupture of the balance between the immunity of the intestinal mucosa and the commensal intestinal flora.
The origin of these failures in the responses of the intestinal immune system is not entirely known, but it is believed to be due to genetic alterations. These can be transmitted to the descendants of patients with UC. However, UC is not considered a hereditary disease in the strict sense. Between 8 and 14% of patients with Ulcerative Colitis have a family history of inflammatory bowel disease. But its manifestation is also influenced by external factors.
Other studies have focused on environmental factors, such as tobacco.
Risk factors that favor the appearance of ulcerative colitis
According to the latest studies, the incidence of ulcerative colitis is between 7 and 10 cases per 100,000 inhabitants2. In fact, it is more prevalent in developed countries with an industrialized lifestyle. Moreover, a study published by the American Journal of Gastroenterology in 20193 shows that people, especially children, who have lived in rural areas have a lower risk of suffering any IBD.
On the other hand, age is a risk factor that influences the appearance of this inflammatory disease. Although the pathology can appear at any age, there is a higher prevalence of ulcerative colitis in the population between 15 and 30 years old. Besides, an increasing number of cases are being diagnosed among children between the ages of 7 and 12. What is the reason? It is probably due to lower exposure to infections during childhood4 and as a consequence the immune system of the intestinal mucosa has poor maturation.
Race or ethnic origin is another risk factor that favors the appearance of ulcerative colitis: white people, especially those with Jewish ancestry of European origin, are more likely to suffer from ulcerative colitis: 5 times more than any other ethnic group.
Diet, NSAIDs and tobacco, do they influence the onset of the disease?
Until a few years ago it was believed that the diet a patient had led during his life could be the cause of the development of an Inflammatory Bowel Disease. But no scientific evidence of it has been found. However, diet can help reduce symptoms and their intensity when the patient has been diagnosed and has a relapse.
The use of drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) is not associated with the onset of ulcerative colitis or with relapse, although some patients have experienced relapses after using them. Therefore, it is essential to be cautious with taking these medicines. It is always necessary to consult with a medical professional.
For its part, tobacco is directly linked to the development of IBD. In fact some studies claim that tobacco is a protective factor against ulcerative colitis5. So much so, that the evolution of the disease in smokers with ulcerative colitis is more moderate compared to that of non-smokers. Even in those who stop smoking, the activity of ulcerative colitis increases. It should not be forgotten, however, that tobacco causes other types of disease, so its use is really not recommended.
- https://www.educainflamatoria.com/cual-es-la-causa-de-la-enfermedad
- https://www.mscbs.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/VOL93/ORIGINALES/RS93C_201903013.pdf
- https://journals.lww.com/ajg/Abstract/2017/09000/Rural_and_Urban_Residence_During_Early_Life_is.16.aspx
- https://www.educainflamatoria.com/que-factores-pueden-influir-en-el-curso-clinico-de-la-enfermedad
- https://www.siicsalud.com/dato/resiic.php/87568
News
Aspects to be taken into account when travelling with ulcerative colitis
July 28, 2022
Patient

Suffering from an inflammatory bowel disease like ulcerative colitis1 does not need to an obstacle to travelling. Some patients may perhaps think that doing this type of travelling carries more risks than needed, but nothing could be further from the truth. Good planning performed with the help of the medical professionals in charge of the patient is the best option for travelling peacefully.
The best time for taking a trip, whether for business or leisure, is when they are in remission. Hence the need to find a treatment that has a longer relapse-free period and where applying a systemic maintenance therapy is no longer needed. Studies2 were performed on leukocyte apheresis3 a few years ago that showed the efficacy of this method, providing an average duration of clinical remission of around 10 months (Ljung et al 2007)4.
Taking this into account, and even though the remission rates and duration differ depending on each patient profile, selective granulocytoapheresis (GMA) has been shown to be an effective tool for inducing clinical remission in patients with ulcerative colitis. For that reason, it is a part of the healthcare professional’s therapeutic arsenal for improving the quality of life of patients with ulcerative colitis.
What must be taken into account with respect to drugs for treating ulcerative colitis?
Even though the period of clinical remission has been increased thanks to leukocyte apheresis treatment, the patient sometimes needs to go travelling when they are suffering a flare-up, or a relapse may even start during the trip itself.
In such cases, patients that are going to travel need to take a few precautions regarding the drugs they are using to treat their disease. For example, taking extra drugs is recommended in case of unforeseen circumstances, keeping them in the original packaging to make them easier to identify, and it is recommended to take 2-3 days’ worth of medicine in cabin luggage if travelling by air.
On the other hand, when biologics have to be taken, these should be carried in a cooler bag with refrigerants so that the cold chain remains unbroken.
It is also advisable to take anti-diarrhoeal and antispasmodic drugs, oral rehydration solution (ORS), analgesics and even antibiotics for cases where the traveller has diarrhoea or fever with bloody stools. If no ORS is available, a substitute mixture of 1 litre of bottled water, 6 tablespoons of sugar and 1 tablespoon of salt can be made.
Documentation the patient should carry regarding their disease
One of the essential documents the patient should carry on them is an updated medical report where the generic names for their drugs are included, especially if they are immunosuppressive (corticosteroids, azathioprine, mercaptopurine, methotrexate) or biological treatments. This document is mandatory if the patient is travelling by air as proof of the drugs they are carrying in their hand luggage, so that no problems arise when accessing it. Furthermore, it is advisable that the report be written in English when travelling abroad.
It is also advisable to take drug prescriptions that contain the patient’s full name and surname and their date of birth; the prescription’s issue date; details of the doctor prescribing the drug (name and surname, contact details, license number, specialisation, address and signature); and the details of the prescribed drug (active ingredient, amount, daily dose, regimen, pharmaceutical form and brand name).
Additionally the patient can ask their doctor to prepare an emergency action plan in case they suffer a flare-up during the trip or the disease worsens.
Other documentation that is recommended to always carry on them whilst travelling with ulcerative colitis is the contact number for the doctor treating the patient, their health card (Spanish if it is a domestic trip or European if the destination is a country within the European Union) and the receipt for health insurance purchased for trips abroad covering healthcare in the country they are travelling to. And. specifically, insurance covering possible issues linked to Inflammatory Bowel Disease.
Other aspects to be taken into account when travelling with ulcerative colitis
Recommendations that the patient must consider adopting a preventive attitude in terms of food whilst travelling. Namely, drinking bottled water, boiled or treated for drinking and brushing teeth; not having ice in drinks; avoiding raw food (like vegetables, salads, etc.); not ingesting street food; or peeling fruit. All of this aimed at avoiding a flare-up of ulcerative colitis or a deterioration.
Additionally, emphasis is placed on the importance of locating bathrooms whilst travelling. Especially so the patient feels more confident. To this effect, there are countries like Great Britain where it is easier to find public bathrooms thanks to applications like The Great British Public Toilet Map5, which is very useful for patients with ulcerative colitis and Crohn’s disease, as well as for the general public.
They have also published the IBD Passport6 website (available in Spanish) in this country where travellers with inflammatory bowel disease (IBD) can find further advice and information on the disease.
And if patients with ulcerative colitis need any type of help, they can get in touch with the patient associations that participate in the EFCCA7, the European Federation of Crohn’s & Ulcerative Colitis Associations, whether they are in Spain or in other countries8.
Lastly, they should not forget to ask their doctor about vaccination recommendations9 if they are going to travel to Asian, South American or African countries. Furthermore, if there is a high probability of contracting yellow fever in said country, it is not advisable for the patient to travel to this destination10.
- What is ulcerative colitis? – Adacyte
- https://www.aegastro.es/publicaciones/publicaciones-aeg/protocolos-asistenciasles-prodiggest/uso-racional-de-la-granulocitomonoaferesis-en-la-enfermedad-inflamatoria-intestinal
- Adacolumn® – Adacyte
- https://www.aegastro.es/publicaciones/publicaciones-aeg/protocolos-asistenciasles-prodiggest/uso-racional-de-la-granulocitomonoaferesis-en-la-enfermedad-inflamatoria-intestinal
- https://www.toiletmap.org.uk/
- https://www.ibdpassport.com/
- https://www.efcca.org/
- http://www.efcca.org/en/members
- http://www.vivirconeii.es/viviendo-con-eii/el-estilo-de-vida-importa/viajes
- https://www.mscbs.gob.es/profesionales/saludPublica/sanidadExterior/salud/viajesInter/home.htm
News
How to act in case of an outbreak of ulcerative colitis?
July 12, 2022
Patient

To what extent can an outbreak of ulcerative colitis interfere with my future plans? Will those outbreaks have implications for my social and family relationships? What about my professional achievements? What can I do when they show up? These are some of the questions that concern people who are diagnosed with ulcerative colitis. And that is because, although today these patients can have a good quality of life, it is inevitable that they worry about the moments when the symptoms of their illness are activated. That is because their expectations and quality of life will be altered.
To understand what an outbreak is, it is important to know that ulcerative colitis will be silent at many times. In other words, the patient will have remission periods1. However, at other times, the patient will experience abdominal pain, diarrhea, blood in the stools or a sense of urgency.These symptoms warn of a possible outbreak of ulcerative colitis. Depending on the intensity of the outbreak, other systemic symptoms, also called extraintestinal manifestations (EIM), that affect organs and tissues throughout the body, may appear.
Knowing how to act in case of an outbreak of ulcerative colitis is very important to stop the intensity and duration of the episode. The first step will always be to follow the recommendations of our healthcare professionals at all times. They will ensure to handle our case in an effective and personalized way. In addition, we will be conveyed the recommendations at the level of hydration, nutrition, physical exercise, stress and medication that we need. Below we provide some of these tips.
Hydration in outbreaks of ulcerative colitis
Diarrhea is an intestinal disorder that alerts the patient to possible dehydration. This is when we can suspect that the patient is suffering a relapse. In this situation, it is essential to act calmly so as not to increase the intensity of the outbreak.
Some tips for treating diarrhea are:
- Increase water intake: it can be bottled, boiled or treated.
- If diarrhea persists for more than one day, it is recommended to take oral rehydration salts (ORS) or, otherwise, a substitute made from 1 liter of bottled water, 6 tablespoons of sugar and 1 tablespoon of salt.
- If the diarrhea lasts for more than three days and is accompanied by fever, vomiting and blood in the stool, the patient should see a doctor or visit the appropriate inflammatory bowel disease unit.
- Under no circumstances should medications to stop diarrhea be taken without medical supervision.
Stress influences outbreaks of ulcerative colitis
Stress is not considered a cause of ulcerative colitis, but it can be the trigger for more serious psychological disorders such as depression and anxiety. In fact, these are identified as two of the most prevalent psychological disorders among patients with Inflammatory Bowel Disease (IBD). Some studies have shown that stressful situations or traumatic life events can exacerbate an ulcerative colitis that is in remission. In other words, stress increases the chances of an outbreak2.
In particular, some of the concerns the patients have are: fecal incontinence and the feeling of urgency, fear of having a new crisis, anticipative anxiety of experiencing some episode in public or not performing well at work or academically, among others.
The reverse can happen too: an outbreak of ulcerative colitis may lead to depression or anxiety. In particular, it is estimated that, in active periods (outbreaks) of the disease, these problems can affect 80% of patients3.
In these cases psychological intervention is one of the pillars in the treatment of ulcerative colitis4. By offering tools to adapt to the disease and the new situation, adherence to pharmacological treatment and assistance to controls is favored. Thus, professionals positively influence the reduction of stress and the improvement of the quality of life of patients with ulcerative colitis.
Physical exercise and ulcerative colitis
Leading a healthy lifestyle helps reduce the stress and anxiety caused by the illness itself. They are also important in order to maintain a good functioning of the intestines, and to strengthen bones and muscles. For this reason, walking, swimming, cycling, practicing pilates or yoga, and even doing exercises at home are more than advisable, both in a situation of remission and relapse.
Diet to follow in case of outbreak
For patients with ulcerative colitis in remission, the diet should be as varied and balanced as possible. However, those who suffer an outbreak must modify their diet5 by reducing the intake of:
- Fiber: whole grains and fresh fruits and vegetables. They should not be completely removed from the diet. They can be consumed baked, steamed or roasted. Basically, the goal is to reduce the chance of having diarrhea and stomach cramps.
- Saturated fats and sugar.
- Lactose-containing foods, mainly milk. Its use can be a cause of worsening of symptoms in periods of inflammatory activity. Nevertheless, it is advisable to maintain the intake of dairy products such as yoghurts, which are better tolerated because the milk is fermented.
On the other hand, for patients with weight loss or who suffer from growth and pubertal development retardation it is advisable to lead a hypercaloric diet.
- Remission of inflammatory diseases – Adacyte
- https://www.sciencedirect.com/science/article/pii/S1873994608000044
- https://www.sciencedirect.com/science/article/pii/S0716864019300781#bib0060
- https://educainflamatoria.com/bienestar-y-apoyo-emocional/como-afecta-la-enfermedad-inflamatoria-intestinal-a-mi-bienestar-emocional/
- Five keys to a proper diet if you have ulcerative colitis – Adacyte
News
The challenge of treating children with ulcerative colitis: when the balance between efficacy and safety is of particular importance
June 16, 2022
Patologies

- Dr. Martín de Carpi is leading a study to assess the efficacy of granulocytapheresis (GMA) in reducing the risk of loss of response to other ulcerative colitis drugs in paediatric patients.
- GMA is the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis.
Madrid, May 2022. Although ulcerative colitis is not a common disease, if we compare it to other childhood-onset digestive diseases, it also affects the paediatric population. In fact, “this chronic disease has experienced a significant increase in incidence in children and adolescents in recent years”. So says Dr Javier Martín de Carpi, gastroenterologist at Sant Juan de Déu Hospital in Barcelona and chairman of the Spanish Society for Paediatric Gastroenterology, Hepatology, and Nutrition (SEGHNP).
This rise in cases has led to the disease being increasingly present during consultations with the paediatric gastroenterologist. In recent years, these cases are diagnosed increasingly earlier and early treatment is introduced, with all the advantages that this entails. Nevertheless, approaching this inflammatory bowel disease continues to be a challenge for the specialist. The paediatric gastroenterologist must achieve a perfect balance between efficacy and safety in the treatment he recommends to the patient.
The doctor highlights a fact that must be taken into account when choosing individualised treatment: the child is going to require treatment for very long periods of their life. However, in addition to checking that this safety profile can be maintained over time, the need to preserve certain biological processes, such as psychological growth, development and maturation, must also be assessed. “It is in our interest that these processes are not affected by the disease on its own or by the treatments that we introduce. Therefore, the approach should control inflammation and its effects rapidly, safely, and in a sustained manner. That way, we are not only taking into account that the treatment is truly effective. It is essential that it is well-tolerated and safe, and that the patient accepts and tolerates it adequately”, emphasises the paediatric gastroenterologist. Dr de Carpí warns that “some drugs can have a negative impact on children’s growth if used for a prolonged period of time (such as steroids), and others whose mechanism of action (control and alteration of the body’s defensive response and its consequences on the intestine) can determine adverse events regarding a higher risk of infections or even long-term tumours, which are fortunately uncommon”.
Granulocytapheresis: efficacy and safety
Dr. Martín de Carpi is currently leading the GUITART study: Granulocyte and monocyte/macrophage apheresis added to infliximab in paediatric patients with steroid- refractory ulcerative colitis to assess [sic] the efficacy and safety of the combined treatment, an investigation to assess the efficacy of granulocytapheresis (GMA) in reducing the risk of loss of response to other drugs. Specifically, it is infliximab biological treatment. “Infliximab is highly effective but unfortunately loses its efficacy over time in a significant percentage of patients”, he explains.
Furthermore, he is the author of the recent publication: Granulocyte and monocyte/macrophage apheresis in paediatric patients with ulcerative colitis: a case series in Spain, in a prestigious medical journal in which he presents his experience using GMA in different patient profiles in clinical practice and the results obtained, both in terms of efficacy and safety. He also details the multiple immunomodulatory effects of GMA that lead to a reduction of intestinal inflammation.
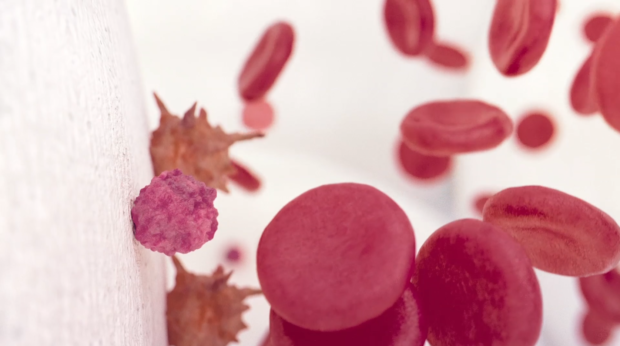
GMA is a non-pharmacological procedure for the treatment of ulcerative colitis (among other immune-mediated diseases). It is the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis. This treatment involves the selective removal of activated neutrophils and monocytes from the bloodstream by passing the patient’s blood through an external column, encouraging their replacement by immature (non-activated) granulocytes and monocytes. This action reduces the migration of these cells to areas of inflammation in the colon, which in turn reduces inflammation in the tissue. In addition, passage through the column induces the secretion of anti-inflammatory cytokines, replacing the inflammatory cells retained in the column with immature cells of anti-inflammatory phenotype. Additionally, apoptotic neutrophils and monocytes returning to the bloodstream trigger the proliferation of anti-inflammatory regulatory T and B cells. All these actions induce an immune reset for an anti-inflammatory phenotype in the patient’s immune system.
The specialist mentions that “as the physician involved in treating these patients, the important thing to bear in mind is that some benefit can be found in each treatment”. He highlights that GMA “has proven its efficacy in different clinical scenarios and exhibits an excellent safety profile. It does not alter the patient’s immune response or other physiological processes inadequately. Furthermore, it allows the possibility of individualising treatment in terms of the technique’s frequency and duration throughout follow-up. Finally, it is a very well-tolerated technique without any relevant adverse events. The technique’s characteristics obviously require access to veins of sufficient size so that it can be performed in adequate conditions. And this is not always easy in children. It is necessary to assess each patient before prescribing and performing it”. In expert opinion, there is another advantage that promotes good adherence and acceptance of the technique: “Given the technique’s “friendly” nature (equivalent to “cleaning and purifying” blood, removing and replacing cells that act by attacking the intestine), provides added reliability and safety for the patient, which makes them trust it and its effects”.
About Adacyte
Adacyte Therapeutics is a pioneering multinational enterprise whose central headquarters is located in Barcelona. It is committed to developing and marketing unique health technologies designed to improve the health and quality of life of patients. It has been operating in Europe since 2018 and its products are currently available in over 150 university hospitals throughout Europe. The company is globally developing Granulocyte-monocyte apheresis (GMA) as a safe and effective treatment option for Inflammatory Bowel Disease (IBD) and other autoimmune diseases.
For more information, visit www.adacyte.com.
News
We solve some of the most frequent doubts after the diagnosis of ulcerative colitis
May 24, 2022
Patologies

When a patient receives the diagnosis of ulcerative colitis many doubts arise around this Inflammatory Bowel Disease (IBD). The main question that patients ask is whether the ulcerative colitis is curable. But that is not the only one. Knowing if they will be able to continue doing their usual life is also one of the major concerns of patients with ulcerative colitis. And because it is a pathology that usually appears in reproductive age, patients in consultations also ask about the possible problems they may have when having children.
In addition, ulcerative colitis does not appear alone. There are other types of manifestations such as the cutaneous ones that appear in relation to the inflammatory disease. That is also a common question. As is the question of where to find truthful and reliable information about the disease. Next we respond to these issues that are of great concern to patients with ulcerative colitis.
Is there a definitive cure for ulcerative colitis?
Ulcerative colitis1 is defined as a chronic disease, which means it is not curable. However, it is controllable thanks to medicines, whichreduce inflammation and heal the intestinal mucosa. In fact, when patients maintain an adequate therapeutic adherence, remission periods2 are prolonged over time. This means that the symptoms of ulcerative colitis disappear for longer periods of time.
Despite proper follow-up and therapeutic compliance, the patient should be aware that, although he will have asymptomatic periods, he will also experience periods with less or more intense outbreaks3. According to some studies, in order to prevent relapses and effectively treat ulcerative colitis, the multidisciplinary approach to the disease is a basic pillar4. In other words, patients will be treated by primary care, gastroenterologists, gastroenterology nurses and psychologists, among other health professionals.
Will the disease affect my quality of life?
After confirming the diagnosis of ulcerative colitis, patients and their families want to know to what extent the pathology will affect their daily lives. When patients relapse, their quality of life will be affected from a physical point of view (abdominal pain, diarrhea, tiredness), from a social point of view (cancellation of social commitments, loss of work) and from a psychological point of view (sadness, anxiety, stress).
But quality of life is a personal and subjective term, so the degree of adaptation to the disease, its treatment and side effects will be decisive in the perception that each patient has of its quality of life.
For example, a patient with certain symptoms, degree of activity of ulcerative colitis and treatment may feel that his quality of life after diagnosis of ulcerative colitis is higher than that of another patient in the same situation.
It is important for the health professionals to know what each patient’s perception of their illness is. Hence a measure such as the so-called Health-Related Quality of Life (HRQOL) is a very helpful tool. Using Quality of Life questionnaires5 we are able to measure, evaluate and know the impact of a disease on the sufferer. In particular, one of the most used for its simplicity is the IBDQ-9 questionnaire6: it consists of 9 questions with 7 possible answers.
Can I have children if I have ulcerative colitis?
Another of the doubts that arise with the diagnosis of ulcerative colitis is related to the patients’ desire to have children. The answer to the question of whether they can have children is yes, a patient with ulcerative colitis can have children. In fact, men and women whose disease is inactive or in remission are just as fertile as the general population. They just need to keep in mind some considerations.
In the case of women, it is recommended to plan the pregnancy and make it coincide with a period of remission to avoid complications such as abortions, preterm births or low birth weight. Besides, with proper monitoring and treatment, the course of pregnancy and childbirth can be fully normal. And the newborn can be healthy.
Obviously, when patients are in an outbreak situation or with an active IBD, fertility is reduced. Among other reasons, it is a consequence of the decrease in sexual desire or the discomfort related to the symptoms of the outbreak itself. Intestinal surgery due to adhesion formation and anatomical abnormalities, as well as removal of the colon, may also affect women’s7 fertility.
What types of skin manifestations are related to this pathology?
One third of IBD-related extraintestinal manifestations affect the mucous membranes and the skin. The most common in patients with ulcerative colitis are pyoderma gangrenosum, erythema nodosum and aphthous stomatitis or mouth ulcers (aphthae)8.
Pyoderma gangrenosum is a non-infectious ulcer that tends to start as a painful nodule or pustule that ulcerates afterwards. It is located mainly in the lower limbs, although it can be located anywhere in the body. This skin lesion is treated locally with corticosteroids, although it improves with the treatment for ulcerative colitis itself. Finally, indicate that it may occur before, during or after an outbreak.
For its part, the erythema nodosum also appears mainly in the lower limbs. It is a lesion characterized by painful, warm reddish-violet subcutaneous nodules. Its appearance is associated with an outbreak of ulcerative colitis. The treatment to tackle the relapse also works to treat the erythema nodosum. Likewise, in order to reduce the skin lesion, it is also recommended to rest keeping the limbs high and, sometimes, to use compressive bandages.
Finally, recurrent aphthous stomatitis is an oral manifestation that may occur before an outbreak of ulcerative colitis. It is characterized by the appearance of small open ulcers on the mucosa of the mouth, circular, whitish in color and with a reddened edge due to inflammation. In this case, they also improve with the patient’s treatment for IBD. Ointments or mouthwashes with anesthetics and/or corticosteroids are used as local treatment.
Where to find reliable information on ulcerative colitis
There is a lot of information circulating on the Internet about ulcerative colitis, but not all of it has a scientific and medical endorsement. In other words, not all of it has truthful, verified and correct information. Therefore, when there is a diagnosis of ulcerative colitis, in addition to taking into account some recommendations to find reliable forums on the disease9 , the patient can visit some sites that do meet the conditions to be properly informed about ulcerative colitis.
In the first place, G-Educainflamatoria10 stands out. It is a space created by the Spanish Working Group on Crohn’s Disease and Ulcerative Colitis (GETECCU), an association created to study and investigate IBD and help improve patients’ lives. Precisely for this purpose they created G-Educainflamatoria, a space aimed at patients where very valuable information about Crohn’s disease and ulcerative colitis is offered.
For its part, the Intestinal Inflammatory Disease Group of the Polytechnic and University Hospital La Fe in Valencia, a multidisciplinary group of health professionals specialized in the care of patients with IBD, has created the IBD La Fe11 space. The aim of this initiative is to serve as a reference for patients with IBD and to provide a place where they can solve their doubts concerning these chronic intestinal diseases.
Finally, the Spanish Digestive System Foundation (FEAD)12 is an institution created by the Spanish Society of Digestive Pathology (SEPD) and supported by more than 2,500 specialists in the Digestive System. In their pages patients can find serious and reliable scientific information that helps to improve their well-being and digestive health.
- What is ulcerative colitis? – Adacyte
- Remission of inflammatory diseases – Adacyte
- Ulcerative colitis and Crohn similarities – Adacyte
- https://www.elsevier.es/es-revista-enfermedad-inflamatoria-intestinal-al-dia-220-articulo-colitis-ulcerosa-remision-mejora-adhesion-S1696780116300288
- https://telecumple.educainflamatoria.com/calidad
- https://telecumple.educainflamatoria.com/q2
- http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-01082007001100011
- https://www.elsevier.es/es-revista-piel-formacion-continuada-dermatologia-21-articulo-manifestaciones-cutaneas-enfermedad-inflamatoria-del-13090362?code=yiS3gXmZwDP2McQq14JkhHOKes7oW9&newsletter=true
- Forum on ulcerative colitis – Adacyte
- https://www.educainflamatoria.com/
- https://eiilafe.com/
- https://www.saludigestivo.es/
News
GEDII 2021
October 19, 2021
Events

For the annual congress of the Portuguese Inflammatory Bowel Disease Study Group (GEDII 2021), Adacyte Therapeutics went to Porto to share its experiences in ulcerative colitis and Crohn’s disease.
From 22nd to 24th September Adacyte was able, in contact with doctors from different countries, to exchange and share their experience and knowledge about new treatments for Crohn’s disease and ulcerative colitis. Adacyte, loyal to its commitment to patient’s health, has continued to work hard during this congress to promote Adacolumn®. We tried our best to show Portuguese experts in IBD the existing real-world evidence of the Adacolumn® beneficial effects in reduction of inflammation and remission of the disease. Adacolumn® is a unique non-pharmaceutical treatment using therapeutic granulocyte and monocyte apheresis, whether in terms of efficacy or safety.
Highlights of the GEDII Congress
On the morning of the first day of the congress, a training session was held on the procedure for publication in scientific journals in which many young doctors participated. It was then followed by an advanced course in IBD monitoring with biomarkers.
In general, during the second day the scientific program was very complete with a review of interesting topics such as imaging techniques, the establishment of quality standards, IBD complications and new treatments.
News
World IBD day, May 19th, 2021
May 17, 2021
Events
Granulocyte and monocyte apheresis shows a differential mechanism of action and excellent efficacy and safety in managing ulcerative colitis.
- Given the unmet need for safer therapeutic alternatives for treating ulcerative colitis, granulocytapheresis has proven its efficacy in different clinical settings and shows an excellent safety profile.
- Dr. Eugeni Domènech, Head of the Digestive System Department at the Germans Trias i Pujol University Hospital in Badalona, is one of the authors of the article, which updates the GMA mechanism of action, recent clinical data on efficacy and safety, and practical aspects of the use of GMA in patients with ulcerative colitis from a European perspective.
Madrid, May 2021. Half of all patients with ulcerative colitis (UC) require at least one course of systemic corticosteroids in their lifetime. Approximately 75% of these patients will also need immunosuppressive drugs in the medium term to avoid colectomy. These drugs raise concerns about the increased risk of serious and opportunistic infections and cancer, especially in older patients and those with comorbidities, highlighting the unmet need for new and safer therapeutic alternatives to manage them.
Granulocyte and monocyte apheresis (GMA), a non-pharmacological procedure (CE-marked medical device) for the treatment of ulcerative colitis (among other immune-mediated diseases), remains the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis. This treatment involves the selective removal of activated neutrophils and monocytes from the bloodstream by passing the patient’s blood through an external column, encouraging their replacement by immature (non-activated) granulocytes and monocytes. This action reduces the migration of these cells to areas of inflammation in the colon, which in turn reduces inflammation in the tissue. In addition, passage through the column induces the secretion of anti-inflammatory cytokines, replacing the inflammatory cells retained in the column with immature cells of anti-inflammatory phenotype. Additionally, apoptotic neutrophils and monocytes returning to the bloodstream trigger the proliferation of anti-inflammatory regulatory T and B cells. All these actions induce an immune reset for an anti-inflammatory phenotype in the patient’s immune system.
In fact, this procedure has proven its efficacy in different clinical scenarios and exhibits an excellent safety profile. It is therefore a first-line therapy in Japan. However, although the treatment has been approved by the European Union since the early 2000s, it is used differently in our environment.
Use of GMA: Mechanism of action, efficacy and practical aspects
The aim of the article “Use of granulocyte/monocytapheresis in ulcerative colitis: a practical review from a European perspective” was to provide an overview of recent clinical data on GMA, its efficacy and the practical aspects of its use in ulcerative colitis from a European perspective. The article was published in the March issue of the prestigious World Journal of Gastroenterology. Among the main results, it is established that GMA is a well-tolerated treatment, with excellent patient perception, and that it also offers the possibility to treat the disease using a unique mechanism of action that compliments other drugs approved for the management of UC.
“The emergence of biological treatments for UC from 2005 onwards initially reduced interest in GMA. However, these drugs have limited efficacy in the medium term, with clinical remission rates at one year of around 30% of treated patients, a high probability of secondary loss of response and, in the case of anti-TNFs, a suboptimal safety profile. All this has rekindled interest in GMA, both as a rescue treatment and as concomitant treatment with biological drugs, given that it does not increase the risk of adverse effects”, explains Dr. Eugeni Domènech, Head of the Digestive System Department at the Germans Trias i Pujol University Hospital in Badalona and main author of this update.
Dr. Domènech regrets that GMA has become a rescue treatment after anti-TNF drugs in Europe. He calls for GMA to be “an alternative in vulnerable patients (elderly, with severe comorbidities or with a recent history of cancer)”. In addition, it raises the possibility of starting combination treatments with any of the drugs currently available in order to increase short-term efficacy.
For the future, and in the absence of robust studies to prove it, he predicts that GMA “could be a strong candidate for preventive treatment of new flares-up in at-risk patients, without increasing the risk of adverse effects of treatment”. The doctor argues that although multiple studies have been carried out over the last decade evaluating genetics, genomics (mRNA, microRNA), proteomics and even metabolomics, as well as studies based on the gut microbiota, to identify biological pathways or new therapeutic targets, the results obtained so far do not yet permit us to identify which treatments are most suitable for each patient or at each moment in time.
News
Ulcerative colitis and Crohn similarities
December 17, 2020
Patologies

Crohn’s diseases and ulcerative colitis: similarities and differences
It occurs with diseases as common as the flu and the cold. It also occurs in neurodegenerative pathologies such as Alzheimer’s and senile dementia, or in psychiatric conditions such as schizophrenia or bipolar disorder. They are different concepts; however, as they are closely related because they have common symptoms, they belong to the same clinical specialty or they are located in the same organ of the human body, they are often confused with each other. The Inflammatory Bowel Disease (IBD) is not an exception. Crohn’s disease and ulcerative colitis are diseases that people tend to confuse.
Knowing the similarities and differences between Crohn’s disease and ulcerative colitis not only is key to the patient. Having rigorous and detailed information is essential for everyone around him. The former will handle better his disease improving his quality of life. The latter will achieve the capacity of empathize with the patient to understand his vision of the reality, his opinions and his doubts by stablishing that bond so demanded of respect and understanding.
Shall we talk about the distinct symptoms of Crohn’s disease and ulcerative colitis? Do we find differences in the characteristics of the inflammation or the damages? What extra-intestinal manifestations can be detected in each one? Are there differences in the way those diseases occur?
Differences between Crohn’s disease and ulcerative colitis
When we talk about Inflammatory Bowel Disease (IBD), we refer to a set of chronic diseases that occur through outbreaks and in which the digestive tract may be affected. If the affectation occurs in the colon, we would be talking about ulcerative colitis. But, in the case of Crohn’s disease, it can be detected anywhere else in the digestive tract.
Although the main difference lies in the affected area, there are more characteristics unique to each disease: incidence, inflammation, complications, symptoms and blood emission in the stools. For example, its incidence: in Spain ulcerative colitis affects 58% of the population, whereas Crohn’s disease affects 42% of it.
Regarding inflammation, it should be noted that in the case of Crohn’s disease, it affects all layers of the intestine. The inflammation in ulcerative colitis is more superficial. With Crohn’s disease, stenosis and fistulas are observed as complications; whereas in ulcerative colitis these do not occur. We also find differences in the main symptoms that warn of the existence of these diseases and in the emission of blood in the depositions. For ulcerative colitis is the diarrhea and for Crohn’s disease is the abdominal pain. Finally, as far as the release of blood in the stool is concerned, we find that the ulcerative colitis patient usually presents blood in the stool on a regular basis, while the Crohn patient bleeds only if the colon is affected.
Similarities between Crohn’s disease and ulcerative colitis
Crohn’s disease and ulcerative colitis are the two most representative pathologies in IBD. When we speak of Crohn’s disease or ulcerative colitis we refer to inflammatory, chronic pathologies caused by a failure in the immune system. Both disrupt food digestion and nutrient absorption. Their cause is unknown, but it is known that genetic factors and other environmental factors are combined. Another common issue is that neither has a cure.
Crohn’s disease and ulcerative colitis resemble according to the profile of the patient in which they occur, the course of the disease, the appearance of extra-intestinal manifestations and the symptoms.
Both tend to manifest themselves at a young age, with an average diagnosis around the age of 30. Half of the patients are between 20 and 40 years old and only 25% have IBD before the age of 20. Regarding gender, women and men are equally likely to suffer from these pathologies. This possibility is slightly greater for men in the case of ulcerative colitis and for women in Crohn’s disease.
It is common in both diseases to occur with periods of activity (outbreaks) and others of remission. Their extra-intestinal manifestations are another similarity. Although they are pathologies exclusive to the digestive system, they can also affect other organs outside it. Rheumatological, dermatological and ophthalmological complications are the most common.
Finally, if there is anything very similar between Crohn’s disease and ulcerative colitis that is their symptoms. Although some occur differently depending on the patient’s IBD, most of them are the same. The most frequent are diarrhea, abdominal pain, fiver, fatigue and anemia. Weight loss and psychological disturbances, especially the lowering in the person’s self-esteem, are also common. Finally, the stunting in growth and sexual maturation of children and adolescents are common symptoms too.
News
What is ulcerative colitis?
November 17, 2020
Patologies

Ulcerative colitis is an intestinal inflammatory disease that starts in the rectum and spreads out to all the sections of the colon (ascending, transverse and descending). It is a chronic disease that results in inflammation in the wall of the large intestine, known as mucosa, which works as a barrier against harmful substances and helps with secreting and carrying nutrients, water and minerals. At times, the inflammation of the mucosa extends to another layer of the colon which causes the wall to get thinner. That contributes to the likelihood of its perforation. Just like in Chron’s disease, ulcerative colitis (UC) presents periods of activity and others of remission.
UC causes the excessive apparition of ulcers, mucus and blood on the inside surface of the intestine. Those ulcers usually happen to be little and superficial. However, if they spread, they generate an accumulation of inflammatory cells. When those wounds heal, they may cause the apparition of little masses of tissue.
Besides, UC may affect other parts of the body like eyes, skin, joints… what is known as extraintestinal manifestations. That makes the patient suffer from joint pain, skin spots, stones in the gallbladder, or eye inflammation.
Just as the cause of the disease is unknown, there is no cure for it either. Nevertheless, if the symptoms are too injurious and the treatments do not work effectively on the patient, surgery may be done. It consists of reconstructing the intestinal transit with a reservoir. Another option is to remove the colon. That is considered to be the cure for the UC. Notwithstanding, it only happens after the failure of every other treatment. It is individually studied in every patient, in cases of extreme necessity.
What is the cause of ulcerative colitis?
UC arises as a consequence of a poor immune response to the organism itself. The origin of this inappropriate response is still unknown, but the stronger theories point at the genetic predisposition, the bacterial flora and the environmental influences as the possible causes of the disease.
There exist multiple harmful substances to our intestine, to which the immune system (under normal circumstances) responds properly protecting the organism from any damage that may affect it. Sometimes those intestinal immunologic responses fail and that is when the UC appears. This situation is usually prolonged and maintained in the long term, making the ulcerative colitis a chronic disease.
The reasons why those immune responses fail are still unknown, but the most powerful theories state that it could be due to genetic alterations of the intestinal immune system. Its cells have the ability to notice the presence of different pathogenic agents and they are able to stop them. Some people present genetic alterations in those agents’ receptors, which lead to wrong identifications and, consequently, to wrong inflammatory responses.
Is the ulcerative colitis hereditary?
Despite the implication of genetic factors in the apparition of the disease, it is not considered to be hereditary. That is because the external factors like tobacco, the previous gastrointestinal infections, some drugs, or even the stress have influence on it too. It does exist the hereditary influence in suffering from UC. However, it is not more than 15% of the risks for first-degree relatives.
How is ulcerative colitis diagnosed?
Diagnosing the disease is sometimes difficult, because the symptoms may be diverse and, in some occasions, they are attributed to other conditions. The blood and stool tests are the most reliable ones, they can help identify if there is inflammation or infection; the so-called image tests, where the inflamed zones may be seen, besides the extension and the seriousness of the disease. And lastly, the endoscopic tests with biopsies confirm the diagnosis of the UC. Those provide any type of necessary information in order to know if there exist ulcers, inflammation, bleeding or stenosis.
Ulcerative colitis1 is an intestinal inflammatory disease that affects the colonic mucosa (large intestine). This mucosa works as a barrier against harmful substances. It also helps secreting and transporting nutrients, water and minerals; and lubricating the inner part of the intestine in order to facilitate defecation. Its inflammation is produced because the immune system generates an inappropriate inflammatory response against the organism itself. The origin of this failure in the intestinal immune system’s responses is not fully known.
When the mucosa gets inflamed, little wounds (ulcers) appear in the inner lining of the colon. This chronic inflammation starts in the rectum and spreads out to other sections of the colon (ascending, transverse and descending). That means that the affectation may have a variable extension.
The most common symptoms of the ulcerative colitis are liquid defecations with mucus and/or blood, stomach ache, straining to defecate, fever, weight loss and fatigue. Besides, other organs like skin, eyes, bones, etc. may be affected. Most people suffering from ulcerative colitis experience from mild to moderate symptoms. There will be periods of activity when the symptoms occur (called flares). However, there are also periods of normality when the disease seems to disappear (called remission phases). Some people may experience long remission phases.
Risk factors As well as Crohn’s disease, UC is a modern age disorder. In fact, the frequency has increased in developed countries since the mid-twentieth century. This disease affects males and females approximately in equal proportions.
The risk factors may be:
- Age. Even though it may appear at any age, it generally occurs before the age of 30. Nevertheless, there are also cases in which the disease has been diagnosed after the age of 60.
- Race or ethnic origin. Although white people have a higher risk of experiencing the disease, any race can have it. If you have Ashkenazi Jewish ancestry, the risk is higher.
- Family history. It is frequent to find UC cases within the members of the same family. Between 8 and 14% of the patients with ulcerative colitis have a family history of inflammatory bowel disease. Therefore, the risk increases when you have a close relative (parent, sibling or son/daughter) who suffers from this disease.
The cause of the ulcerative colitis and other unknown issues for the science Even though science has made great efforts to find out the cause of ulcerative colitis, it is still unknown. Science still wonders what the specific cause of the inappropriate inflammatory response of the immune system is. According to GETECCU2, current researches state that the disease may appear as a result of a complex interaction of several factors.
One of those factors is a person’s genetic predisposition (susceptibility) to suffer from the disease. However, there are other factors that also seem to be the key in the appearance of the UC like the exposition to environmental factors, the intestinal commensal microflora and the possible involvement of infectious agents. It is believed that the genetic alterations affect the ability of the immune system to tolerate the commensal bacteria and the intensity of the inflammatory response against those bacteria.
Nonetheless, the genetic origin is not completely clear yet. In conjunction with this issue, there exist questions about the pathogenesis of ulcerative colitis that still pose a challenge to science. Why is the inflammation restricted to the mucus layer? Are the epithelial cells of the colon the specific aim of an immune response? How does the luminal microbiota affect the inflammatory response?
Contact UsFor more information
Contact Us